The Role Of Gut Health In Hyperthyroidism: Emerging Insights
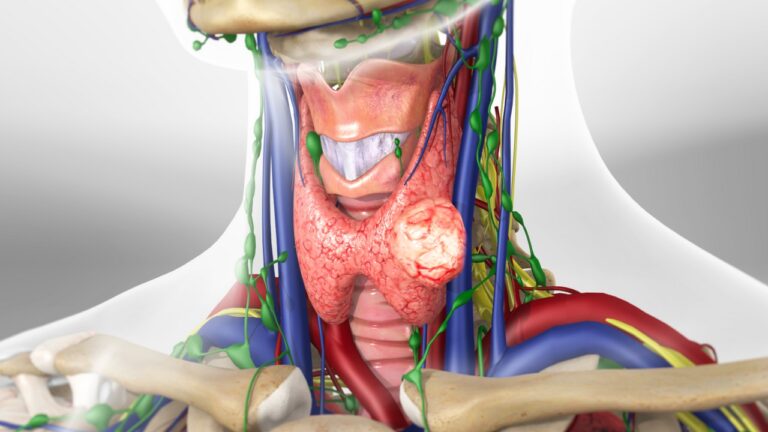
In recent years, researchers have increasingly recognized the intricate interplay between gut health and various physiological processes throughout the body, including thyroid function. Hyperthyroidism, a condition characterized by an overactive thyroid gland, is no exception. Emerging evidence suggests that disturbances in gut microbiota composition, intestinal permeability, and immune responses may influence the development and progression of hyperthyroidism. In this article, we delve into the evolving understanding of the role of gut health in hyperthyroidism, exploring the mechanisms involved and the potential implications for clinical management.
Understanding Gut Microbiota and Thyroid Function
The gut microbiota, comprising trillions of microorganisms inhabiting the gastrointestinal tract, plays a crucial role in maintaining host health and homeostasis. These microbial communities interact with the immune system, modulate metabolic processes, and influence the absorption and metabolism of nutrients and medications. Moreover, emerging research has highlighted the bidirectional communication between the gut and the thyroid axis, suggesting that alterations in gut microbiota composition may impact thyroid function and vice versa.
Several studies have demonstrated associations between gut dysbiosis—an imbalance in gut microbiota composition—and thyroid disorders, including hyperthyroidism. Imbalances in specific bacterial taxa, such as decreased levels of beneficial probiotic species and overgrowth of pathogenic bacteria, have been observed in individuals with hyperthyroidism. These dysbiotic changes may contribute to inflammation, oxidative stress, and autoimmune responses implicated in the pathogenesis of hyperthyroidism.
Impact of Gut Health on Immune Dysregulation
Immune dysregulation is a hallmark feature of autoimmune thyroid disorders, including Graves’ disease, the most common cause of hyperthyroidism. Mounting evidence suggests that the gut microbiota plays a crucial role in shaping immune responses and maintaining immune tolerance. Dysbiosis-induced alterations in gut barrier integrity and mucosal immune function may lead to the translocation of bacterial antigens and trigger aberrant immune responses targeting thyroid tissue.
Moreover, the gut microbiota can influence the differentiation and activation of immune cells involved in thyroid autoimmunity, such as T helper 17 (Th17) cells and regulatory T cells (Tregs). Imbalances in these immune cell populations have been implicated in the pathogenesis of autoimmune thyroid disorders. By modulating immune responses and promoting immune tolerance, interventions targeting gut health may offer novel therapeutic avenues for mitigating autoimmune-mediated hyperthyroidism.
Role of Intestinal Permeability and Endotoxemia
Intestinal permeability, commonly referred to as “leaky gut,” refers to the disruption of the intestinal barrier that regulates the passage of molecules between the gut lumen and systemic circulation. Dysregulation of intestinal permeability has been implicated in various autoimmune and inflammatory conditions, including hyperthyroidism. Increased intestinal permeability allows the translocation of microbial products, such as lipopolysaccharides (LPS) from gram-negative bacteria, into the bloodstream—a phenomenon known as endotoxemia.
Elevated circulating levels of LPS and other microbial-derived toxins can trigger inflammatory responses and activate immune cells, contributing to systemic inflammation and autoimmune reactions. In individuals with hyperthyroidism, heightened intestinal permeability and endotoxemia may exacerbate thyroid autoimmunity and amplify the inflammatory cascade associated with the condition. Targeting intestinal barrier integrity and gut microbiota composition through dietary interventions, probiotics, and prebiotics may help restore gut health and attenuate hyperthyroidism-related inflammation.
Clinical Implications and Therapeutic Strategies
The emerging insights into the role of gut health in hyperthyroidism have significant clinical implications for the management of this condition. Integrating gut-focused interventions into the treatment paradigm for hyperthyroidism may complement existing therapeutic approaches and improve treatment outcomes. Here are some potential therapeutic strategies targeting gut health in hyperthyroidism:
Probiotic Supplementation: The administration of probiotics—live microorganisms with beneficial health effects—may help restore gut microbiota balance and modulate immune responses in individuals with hyperthyroidism. Specific probiotic strains, such as Lactobacillus and Bifidobacterium species, have shown promise in preclinical and clinical studies for their immunomodulatory properties.
Dietary Modification: Adopting a nutrient-rich diet high in fiber, antioxidants, and essential nutrients can support gut health and promote microbial diversity. Certain dietary components, such as fermented foods, prebiotic fibers, and polyphenol-rich foods, may exert beneficial effects on gut microbiota composition and function.
Gut Barrier Support: Strategies aimed at preserving intestinal barrier integrity, such as supplementation with glutamine, zinc, and butyrate—a short-chain fatty acid produced by gut bacteria—may help prevent intestinal permeability and reduce the risk of endotoxemia in individuals with hyperthyroidism.
Stress Management: Chronic stress can disrupt gut microbiota composition and exacerbate inflammatory responses, potentially worsening hyperthyroidism symptoms. Incorporating stress-reducing techniques such as mindfulness meditation, yoga, and relaxation exercises may complement conventional treatment approaches and promote overall well-being.
Conclusion
In conclusion, the emerging understanding of the role of gut health in hyperthyroidism underscores the interconnectedness of various physiological systems within the body. Dysbiosis, intestinal permeability, and immune dysregulation may contribute to the pathogenesis and progression of hyperthyroidism, particularly in autoimmune-mediated forms of the condition. Targeting gut health through dietary modifications, probiotic supplementation, and gut barrier support strategies holds promise as adjunctive therapeutic approaches for individuals with hyperthyroidism. Further research is warranted to elucidate the mechanisms underlying the gut-thyroid axis and to optimize gut-focused interventions for improving clinical outcomes in hyperthyroidism management. By recognizing and addressing the intricate interplay between gut health and thyroid function, healthcare providers can adopt a more holistic approach to the management of hyperthyroidism and enhance patient care and well-being.