Silent Thyroiditis: A Closer Look At Its Characteristics
Thyroiditis encompasses a spectrum of thyroid disorders characterized by inflammation of the thyroid gland. Among its various forms, silent thyroiditis stands out as a unique subtype due to its subtle presentation and distinct characteristics. Despite its name, silent thyroiditis can have significant implications for thyroid function and overall health. In this article, we delve into the intricacies of silent thyroiditis, exploring its clinical features, diagnostic approach, and management strategies.
Understanding Silent Thyroiditis:
Silent thyroiditis, also known as painless thyroiditis or subacute lymphocytic thyroiditis, is an autoimmune condition that affects the thyroid gland. Unlike other types of thyroiditis, such as Hashimoto’s thyroiditis or De Quervain’s thyroiditis, silent thyroiditis typically presents without overt symptoms of thyroid dysfunction, such as palpitations, weight changes, or fatigue. Instead, patients may experience mild discomfort or tenderness in the neck region, which often goes unnoticed or is attributed to other causes.
Characteristics and Clinical Presentation:
The hallmark characteristic of silent thyroiditis is the absence of significant thyroid-related symptoms, hence the term “silent.” However, despite the lack of overt clinical manifestations, several key features distinguish this condition:
- Autoimmune Pathogenesis: Like other autoimmune thyroid disorders, silent thyroiditis is characterized by immune-mediated inflammation of the thyroid gland. Autoantibodies, such as thyroid peroxidase antibodies (TPOAb) and thyroglobulin antibodies (TgAb), may be present, indicating an autoimmune etiology.
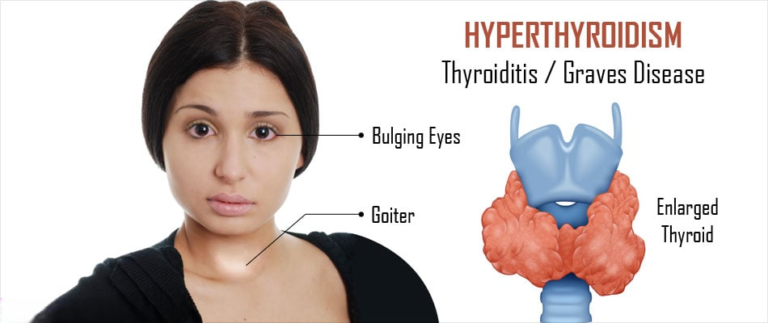
- Transient Thyrotoxic Phase: Silent thyroiditis typically follows a triphasic course, beginning with a thyrotoxic phase characterized by transient hyperthyroidism. During this phase, patients may experience symptoms such as nervousness, heat intolerance, and palpitations, albeit to a lesser extent compared to classical hyperthyroidism. Thyroid hormone levels, particularly free thyroxine (FT4) and triiodothyronine (T3), are elevated, accompanied by low or suppressed thyroid-stimulating hormone (TSH) levels.
- Euthyroid Phase: Following the thyrotoxic phase, thyroid hormone levels gradually normalize, and patients enter a phase of euthyroidism, during which thyroid function returns to baseline. This phase may last for several weeks to months, during which time patients are asymptomatic or experience minimal thyroid-related symptoms.
- Hypothyroid Phase (Optional): In some cases, silent thyroiditis may progress to a hypothyroid phase, characterized by decreased thyroid hormone levels and elevated TSH levels. This phase may occur weeks to months after the euthyroid phase and can manifest with symptoms of hypothyroidism, including fatigue, weight gain, and cold intolerance.
Diagnostic Approach:
Diagnosing silent thyroiditis can be challenging due to its asymptomatic or subclinical nature. However, several diagnostic tests can aid in its identification:
- Thyroid Function Tests: Measurement of serum levels of TSH, FT4, and T3 can help assess thyroid function. In silent thyroiditis, TSH levels are typically low or suppressed during the thyrotoxic phase, normalizing during the euthyroid phase, and may become elevated in the hypothyroid phase.
- Thyroid Autoantibodies: Testing for thyroid autoantibodies, such as TPOAb and TgAb, can support the diagnosis of autoimmune thyroiditis, including silent thyroiditis.
- Thyroid Ultrasound: Ultrasonography of the thyroid gland may reveal characteristic features of thyroiditis, such as diffuse glandular enlargement and heterogeneous echotexture. However, imaging findings are non-specific and may overlap with other thyroid disorders.
Management Strategies:
The management of silent thyroiditis primarily focuses on symptomatic relief and monitoring thyroid function throughout its course. Treatment strategies may include:
Symptomatic Management: During the thyrotoxic phase, symptomatic relief of hyperthyroid symptoms, such as beta-blockers for palpitations or anxiety, may be warranted. Nonsteroidal anti-inflammatory drugs (NSAIDs) can help alleviate neck pain or discomfort.
Monitoring Thyroid Function: Regular monitoring of thyroid function tests is essential to track the progression of the disease and adjust treatment as needed. This includes serial measurements of TSH, FT4, and T3 levels to assess thyroid hormone status.
Avoidance of Iodine: Excessive iodine intake can exacerbate thyroid dysfunction in patients with silent thyroiditis. Therefore, dietary iodine restriction or avoidance of iodine-containing supplements may be recommended.
Endocrine Consultation: Referral to an endocrinologist may be beneficial for comprehensive management, especially in cases of persistent or recurrent thyroid dysfunction.
Prognosis and Long-Term Follow-Up:
In most cases, silent thyroiditis follows a self-limited course, with thyroid function returning to baseline within months of symptom onset. However, a subset of patients may experience recurrent episodes of thyroid dysfunction or progression to chronic autoimmune thyroiditis, such as Hashimoto’s thyroiditis. Long-term follow-up is therefore essential to monitor thyroid function and assess for the development of complications or comorbidities.
Conclusion:
Silent thyroiditis represents a unique variant of autoimmune thyroiditis characterized by its asymptomatic or minimally symptomatic nature. Despite its benign course in the majority of cases, silent thyroiditis underscores the importance of vigilant monitoring and individualized management to ensure optimal thyroid health. By recognizing its characteristic features and employing appropriate diagnostic and therapeutic strategies, healthcare providers can effectively manage this often overlooked thyroid disorder.