Managing Multinodular Goitre: What You Need To Know
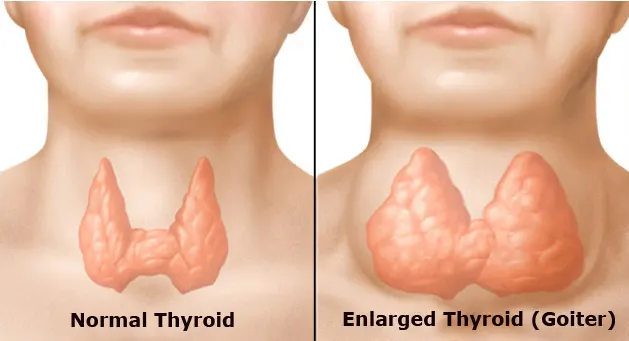
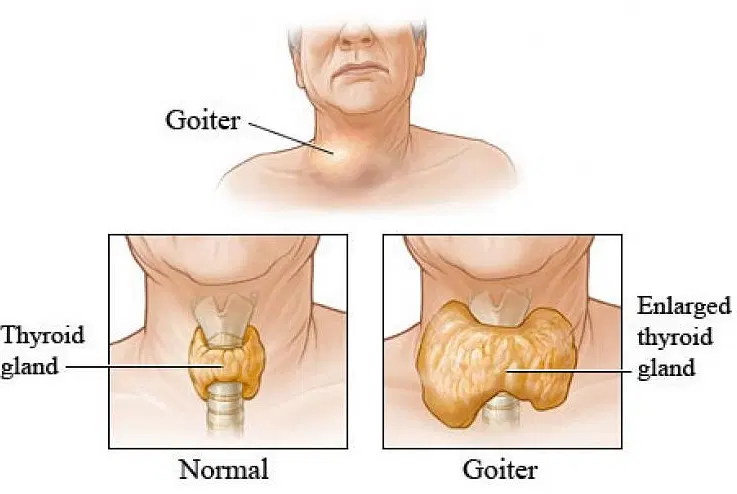
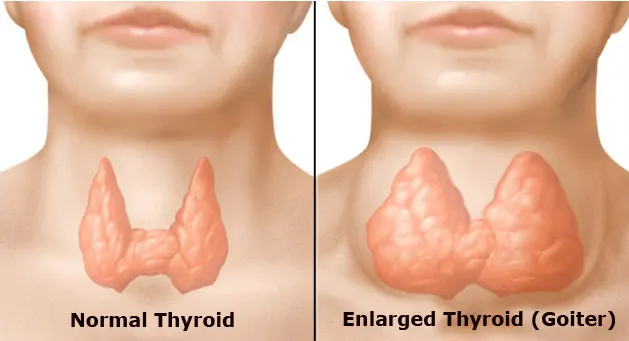
Multinodular goitre (MNG) is a common thyroid disorder characterized by the development of multiple nodules within the thyroid gland. While often benign, MNG can lead to complications such as compression symptoms, thyroid dysfunction, and cosmetic concerns. Effective management of MNG requires a comprehensive understanding of its causes, diagnosis, and treatment options. In this article, we will delve into the key aspects of managing multinodular goitre to provide patients and healthcare providers with valuable insights.
Understanding Multinodular Goitre
Multinodular goitre typically develops due to various factors, including iodine deficiency, genetic predisposition, autoimmune diseases, and environmental influences. The thyroid gland, located in the neck, plays a crucial role in regulating metabolism and hormone production. When nodules form within the thyroid tissue, they can alter its size, shape, and function.
Diagnosis and Evaluation
Diagnosing multinodular goitre involves a combination of clinical assessment, imaging studies, and laboratory tests. Patients may present with symptoms such as neck swelling, difficulty swallowing, hoarseness, or palpitations. Physical examination may reveal an enlarged thyroid gland or palpable nodules. Imaging modalities such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) are utilized to visualize the thyroid gland and assess the characteristics of the nodules. Additionally, thyroid function tests measure levels of thyroid hormones and thyroid-stimulating hormone (TSH) to evaluate thyroid function.
Treatment Options
The management of multinodular goitre depends on several factors, including the size and location of the nodules, symptoms, and the presence of thyroid dysfunction. Treatment options may include:
- Observation: In cases where the nodules are small, asymptomatic, and non-threatening, a watchful waiting approach may be adopted. Regular monitoring through clinical evaluation and imaging studies helps track any changes in the nodules over time.
- Medications: Thyroid hormone replacement therapy with levothyroxine may be prescribed to suppress TSH levels and reduce the size of the goitre. This approach is particularly beneficial for patients with thyroid hormone deficiency or euthyroid multinodular goitre.
- Radioiodine Therapy: Radioactive iodine (RAI) treatment involves the administration of radioactive iodine, which selectively targets and destroys thyroid tissue. RAI therapy is commonly used for the management of hyperthyroidism associated with MNG, aiming to reduce thyroid hormone production and shrink the goitre.
- Fine-Needle Aspiration (FNA) Biopsy: FNA biopsy is a minimally invasive procedure used to obtain tissue samples from thyroid nodules for cytological examination. It helps differentiate between benign and malignant nodules, guiding further management decisions.
- Surgical Intervention: Thyroidectomy, either total or subtotal, may be recommended for patients with large goitres causing significant symptoms, compression of adjacent structures, or suspicion of malignancy. Surgical removal of the thyroid gland can alleviate symptoms, reduce the risk of complications, and provide definitive treatment for MNG.
Considerations and Complications
When managing multinodular goitre, healthcare providers should consider various factors, including patient preferences, comorbidities, and potential complications. Complications associated with MNG include thyroid dysfunction, compression symptoms (such as difficulty breathing or swallowing), cosmetic concerns, and the risk of malignancy. Individualized treatment plans tailored to each patient’s needs and circumstances are essential for optimizing outcomes and minimizing risks.
Conclusion
Multinodular goitre is a common thyroid disorder that requires careful evaluation and management to address symptoms, prevent complications, and ensure optimal patient outcomes. By understanding the underlying causes, utilizing appropriate diagnostic tools, and considering the full range of treatment options, healthcare providers can effectively manage MNG and improve the quality of life for affected individuals. A multidisciplinary approach involving endocrinologists, surgeons, radiologists, and pathologists is often necessary to provide comprehensive care and support for patients with multinodular goitre.