Hyperthyroidism In Pregnancy: Special Considerations And Management
Pregnancy is a time of profound physiological changes, including alterations in thyroid function. Hyperthyroidism, characterized by an overactive thyroid gland, poses unique challenges during pregnancy, as it can impact both maternal and fetal health. In this article, we delve into the special considerations and management strategies for hyperthyroidism in pregnancy, aiming to guide healthcare providers and expecting mothers through this complex condition.
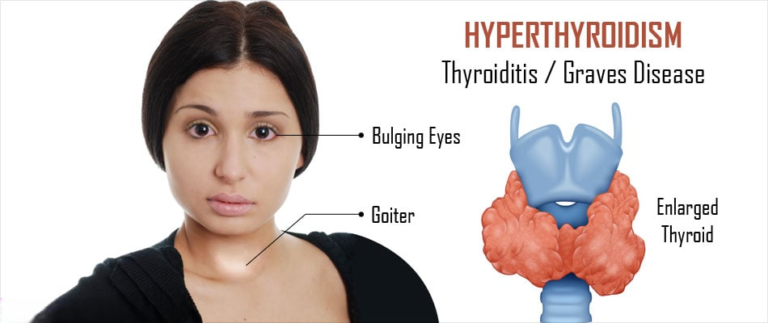
Understanding Hyperthyroidism in Pregnancy
Hyperthyroidism in pregnancy can arise from various etiologies, including Graves’ disease, toxic multinodular goiter, and thyroiditis. Graves’ disease, an autoimmune disorder characterized by the production of thyroid-stimulating immunoglobulins, is the most common cause of hyperthyroidism in pregnancy. The heightened thyroid hormone levels associated with hyperthyroidism can have significant implications for maternal health, fetal development, and pregnancy outcomes.
Special Considerations
- Maternal Health: Hyperthyroidism in pregnancy poses risks to maternal health, including exacerbation of preexisting cardiovascular conditions such as hypertension and tachycardia. Additionally, untreated or inadequately managed hyperthyroidism increases the risk of complications such as preterm labor, preeclampsia, and thyroid storm—a life-threatening hypermetabolic state. Therefore, vigilant monitoring and appropriate management are essential to safeguard maternal well-being.
- Fetal Health: Thyroid hormones play a crucial role in fetal neurodevelopment, particularly during the first trimester when the fetal thyroid gland is not yet fully functional. Maternal hyperthyroidism, if left untreated, can lead to adverse fetal outcomes, including intrauterine growth restriction, low birth weight, and developmental abnormalities. Consequently, optimizing maternal thyroid function is paramount to ensuring the health and development of the unborn child.
Management Strategies
- Preconception Counseling: Women with a history of hyperthyroidism contemplating pregnancy should receive preconception counseling to optimize thyroid function before conception. This may involve adjusting medication dosages, achieving euthyroidism (normal thyroid function), and addressing any underlying autoimmune conditions such as Graves’ disease.
- Antithyroid Medications: Antithyroid medications, such as propylthiouracil (PTU) and methimazole (MMI), are the mainstay of treatment for hyperthyroidism in pregnancy. These medications inhibit thyroid hormone synthesis and are generally considered safe during pregnancy, with PTU preferred in the first trimester due to a lower risk of congenital anomalies. Close monitoring of thyroid function and fetal well-being is essential during antithyroid drug therapy.
- Monitoring: Regular monitoring of maternal thyroid function, including serum levels of thyroid-stimulating hormone (TSH) and free thyroxine (FT4), is crucial throughout pregnancy. Thyroid function tests should be performed approximately every 4-6 weeks to ensure euthyroidism is maintained and medication adjustments are made as necessary. Additionally, fetal growth and well-being should be assessed via obstetric ultrasound and fetal monitoring.
- Multidisciplinary Care: Managing hyperthyroidism in pregnancy often requires a multidisciplinary approach involving obstetricians, endocrinologists, and maternal-fetal medicine specialists. Collaborative decision-making and coordinated care facilitate optimal management and minimize the risk of complications for both mother and baby.
- Radioactive Iodine and Surgery: Radioactive iodine (RAI) therapy and thyroidectomy are generally contraindicated during pregnancy due to the potential risks of fetal thyroid ablation and hypothyroidism. These treatment modalities are typically deferred until after delivery, with alternative management strategies employed to control hyperthyroidism during pregnancy.
Conclusion
Hyperthyroidism in pregnancy presents unique challenges that require careful consideration and management to ensure optimal outcomes for both mother and baby. Through close monitoring, timely intervention, and collaborative care, healthcare providers can effectively navigate this complex condition and mitigate associated risks. By addressing maternal thyroid function and fetal well-being proactively, we can safeguard the health and well-being of pregnant individuals with hyperthyroidism and promote healthy pregnancies and births.