Emerging Therapies In Thyroid Tumor Management: Targeted Treatments
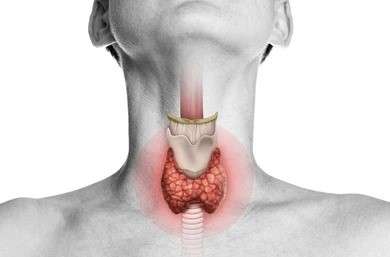
Thyroid tumors, encompassing a spectrum from benign nodules to malignant cancers, pose significant challenges in clinical management. While traditional treatment modalities like surgery, radioactive iodine therapy, and thyroid hormone suppression remain cornerstones, emerging therapeutic strategies are revolutionizing the landscape of thyroid tumor management. Among these, targeted treatments have garnered attention for their potential to offer more precise and effective interventions. In this article, we delve into the concept of targeted treatments for thyroid tumors, exploring the latest advancements, their mechanisms of action, and their impact on patient outcomes.
Understanding Targeted Treatments
Targeted treatments in thyroid tumor management involve therapies designed to selectively interfere with specific molecules or pathways implicated in tumor growth and progression. Unlike traditional chemotherapy, which non-selectively targets rapidly dividing cells, targeted therapies aim to disrupt molecular abnormalities present predominantly in tumor cells, minimizing damage to normal tissues. These therapies often exploit the dysregulated signaling pathways characteristic of thyroid tumors, such as the MAPK and PI3K/AKT pathways, to exert their anti-tumor effects.
Advancements in Targeted Therapies
- Tyrosine Kinase Inhibitors (TKIs): TKIs have emerged as a promising class of targeted therapies for advanced thyroid cancers, particularly those refractory to standard treatments. Drugs like sorafenib, lenvatinib, and vandetanib inhibit multiple receptor tyrosine kinases involved in angiogenesis, tumor growth, and metastasis. Clinical trials have demonstrated their efficacy in improving progression-free survival and even inducing tumor regression in some cases.
- BRAF Inhibitors: BRAF mutations are prevalent in papillary thyroid carcinoma (PTC), driving aberrant MAPK signaling and promoting tumor proliferation. BRAF inhibitors, such as vemurafenib and dabrafenib, specifically target mutated BRAF proteins, leading to suppression of downstream signaling and tumor regression. While initially promising, their efficacy may be limited by acquired resistance mechanisms and the emergence of alternative signaling pathways.
- MEK Inhibitors: MEK inhibitors, including trametinib and cobimetinib, act downstream of BRAF in the MAPK pathway, exerting their anti-tumor effects by blocking MEK-mediated phosphorylation of downstream targets. Combinatorial approaches with BRAF inhibitors have shown synergistic effects in overcoming resistance and improving treatment outcomes in BRAF-mutated thyroid cancers.
- Immune Checkpoint Inhibitors (ICIs): ICIs have revolutionized cancer treatment by unleashing the immune system’s ability to recognize and eliminate tumor cells. Agents targeting programmed cell death protein 1 (PD-1) or its ligand (PD-L1), such as pembrolizumab and nivolumab, have demonstrated efficacy in subsets of patients with advanced thyroid cancers, particularly those with high tumor mutational burden or deficient DNA mismatch repair.
Challenges and Considerations
While targeted therapies offer promising avenues for improving outcomes in thyroid tumor management, several challenges and considerations merit attention.
- Resistance Mechanisms: Tumor cells can develop resistance to targeted therapies through various mechanisms, including secondary mutations, upregulation of alternative signaling pathways, and tumor heterogeneity. Overcoming resistance remains a significant clinical challenge and necessitates the development of novel therapeutic strategies and combination approaches.
- Toxicity Profiles: Despite their specificity for tumor cells, targeted therapies can still cause adverse effects due to off-target effects or interference with essential physiological processes. Common adverse events associated with TKIs include hypertension, fatigue, and gastrointestinal disturbances, underscoring the importance of careful monitoring and management of treatment-related toxicities.
- Patient Selection and Biomarkers: Identifying patients most likely to benefit from targeted therapies remains a critical aspect of personalized medicine in thyroid tumor management. Biomarkers predictive of treatment response, such as BRAF mutation status or PD-L1 expression, can help guide treatment decisions and optimize therapeutic outcomes.
Future Directions
The evolving landscape of targeted therapies in thyroid tumor management holds promise for improving patient outcomes and transforming the standard of care. Future research efforts should focus on elucidating mechanisms of resistance, identifying novel therapeutic targets, and refining patient selection criteria through the integration of molecular profiling and predictive biomarkers. Additionally, combinatorial approaches incorporating targeted therapies with immunotherapy or other treatment modalities represent a compelling strategy for overcoming resistance and enhancing treatment efficacy.
Conclusion
Targeted therapies have emerged as a cornerstone of precision medicine in thyroid tumor management, offering new hope for patients with advanced or refractory disease. By selectively targeting molecular aberrations driving tumor growth and progression, these therapies hold the potential to improve outcomes and prolong survival in subsets of patients. However, ongoing research efforts are needed to address challenges related to resistance, toxicity, and patient selection, ultimately realizing the full potential of targeted treatments in the fight against thyroid cancer.