Advances In Hypothyroidism Research And Treatment
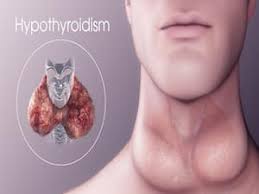
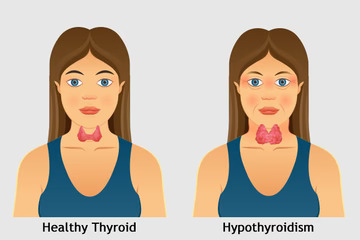
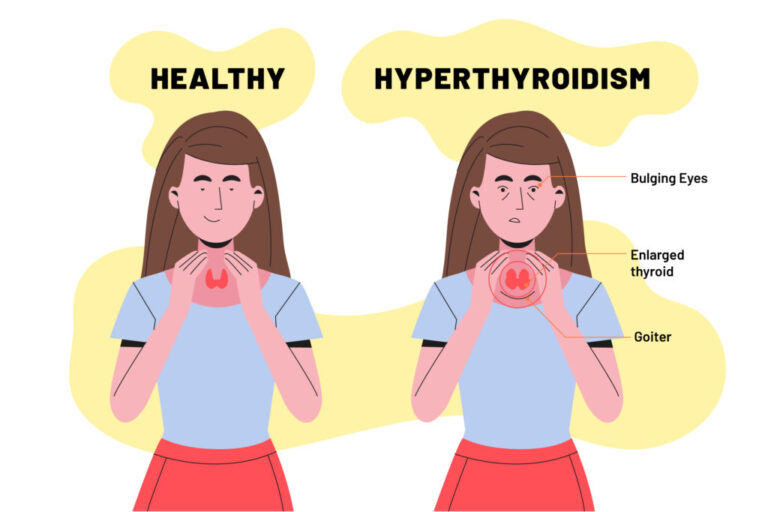
Hypothyroidism, a condition characterized by an underactive thyroid gland producing insufficient thyroid hormones, affects millions of people worldwide. Thyroid hormones are crucial for regulating metabolism, and their deficiency can lead to a variety of symptoms, including fatigue, weight gain, depression, and cognitive impairment. Recent advancements in research and treatment have significantly improved the understanding, diagnosis, and management of hypothyroidism, offering hope for better patient outcomes.
Understanding Hypothyroidism: A Complex Condition
Hypothyroidism can be primary, originating from the thyroid gland itself, or secondary, due to pituitary or hypothalamic dysfunction. Primary hypothyroidism is the most common form and is often caused by autoimmune diseases like Hashimoto’s thyroiditis. Other causes include iodine deficiency, thyroid surgery, radiation therapy, and certain medications.
Researchers have made significant strides in understanding the genetic and environmental factors contributing to hypothyroidism. Genome-wide association studies (GWAS) have identified several genetic loci associated with the disease, enhancing our understanding of its pathophysiology. Furthermore, advancements in immunology have shed light on the mechanisms of autoimmune thyroid diseases, paving the way for targeted therapies.
Diagnostic Innovations
Accurate and timely diagnosis is crucial for effective hypothyroidism management. Traditionally, diagnosis has relied on measuring serum levels of Thyroid Stimulating Hormone (TSH) and free thyroxine (T4). While these tests remain the gold standard, new diagnostic tools and biomarkers are emerging.
One promising area of research is the development of ultrasensitive assays capable of detecting minute changes in thyroid hormone levels. These assays can help diagnose subclinical hypothyroidism, a mild form of the disease where symptoms are not overt but can still impact health. Additionally, advanced imaging techniques, such as high-resolution ultrasound and thyroid elastography, provide detailed insights into thyroid gland morphology and function, aiding in early diagnosis and monitoring.
Advances in Treatment
The primary treatment for hypothyroidism has been hormone replacement therapy, typically using synthetic levothyroxine (T4). While effective for most patients, this treatment requires careful dose adjustment and regular monitoring. Recent advances aim to optimize and personalize hormone replacement therapy.
- Combination Therapy
Emerging evidence suggests that some patients might benefit from combination therapy using both T4 and triiodothyronine (T3). T3 is the active form of thyroid hormone, and in some individuals, supplementing T3 alongside T4 can improve symptoms and quality of life. However, combination therapy remains controversial and requires further research to establish its long-term safety and efficacy. - Personalized Medicine
Personalized medicine is transforming hypothyroidism treatment by tailoring therapy to individual patient profiles. Factors such as genetic variations, age, sex, weight, and comorbidities can influence the optimal thyroid hormone dose. Pharmacogenomics, the study of how genes affect a person’s response to drugs, is gaining traction in hypothyroidism management. By understanding genetic differences in thyroid hormone metabolism and receptor sensitivity, clinicians can better tailor treatments to each patient’s needs. - Novel Drug Formulations
Innovative drug formulations are also being explored to enhance the efficacy and convenience of hypothyroidism treatment. For instance, slow-release T3 formulations aim to provide a more stable hormone level, mimicking the body’s natural secretion patterns. Additionally, liquid and gel-based levothyroxine formulations offer alternative options for patients who have difficulty absorbing traditional tablet forms.
Non-Traditional Therapies
Beyond conventional hormone replacement, researchers are investigating non-traditional therapies to manage hypothyroidism and its symptoms.
- Nutritional Interventions
Nutritional interventions play a crucial role in thyroid health. Iodine, selenium, and zinc are essential for thyroid hormone synthesis and metabolism. Recent studies have explored the benefits of these nutrients in preventing and managing hypothyroidism. For example, selenium supplementation has shown promise in reducing thyroid autoantibody levels and improving thyroid function in patients with autoimmune thyroiditis. - Lifestyle Modifications
Lifestyle modifications, including diet, exercise, and stress management, are gaining recognition for their impact on thyroid health. A balanced diet rich in antioxidants and anti-inflammatory foods can support thyroid function. Regular exercise not only helps manage weight but also improves overall metabolic health. Stress management techniques, such as yoga and meditation, can mitigate the adverse effects of chronic stress on the thyroid gland.
Emerging Therapies and Future Directions
The future of hypothyroidism treatment lies in exploring novel therapeutic targets and developing cutting-edge technologies.
- Thyroid Tissue Engineering
Thyroid tissue engineering is an exciting frontier in hypothyroidism research. Scientists are exploring the possibility of creating bioengineered thyroid tissue using stem cells and 3D printing technologies. This approach could potentially provide a long-term solution for patients with severe thyroid dysfunction or those who have undergone thyroidectomy. - Autoimmune Modulation
For autoimmune hypothyroidism, strategies to modulate the immune system are being actively researched. Monoclonal antibodies targeting specific immune pathways hold promise for reducing thyroid inflammation and preserving gland function. Additionally, advances in immunotherapy, such as checkpoint inhibitors and tolerogenic vaccines, offer hope for preventing and treating autoimmune thyroid diseases. - Artificial Intelligence and Machine Learning
Artificial intelligence (AI) and machine learning are revolutionizing healthcare, including thyroid disease management. AI algorithms can analyze large datasets to identify patterns and predict disease progression, enabling early intervention. Machine learning models can also assist in optimizing hormone replacement therapy by predicting individual patient responses based on their unique characteristics.
Conclusion
Advances in hypothyroidism research and treatment are transforming the landscape of thyroid disease management. From improved diagnostic tools to personalized therapies and cutting-edge technologies, these developments hold promise for enhancing patient outcomes and quality of life. Continued research and innovation are essential to unravel the complexities of hypothyroidism and provide more effective and tailored treatment options for patients worldwide. As the field progresses, the hope is that individuals with hypothyroidism can lead healthier, more fulfilling lives with fewer limitations imposed by their condition.