Advancements In The Treatment Of Multinodular Goitre
Multinodular goitre (MNG) is a common thyroid disorder characterized by an enlarged thyroid gland with multiple nodules. While the exact cause of MNG is often unclear, factors such as iodine deficiency, genetic predisposition, and certain autoimmune conditions are known to contribute. Traditional treatments have included surgical intervention and radioactive iodine therapy, but recent advancements have provided new options that improve outcomes and reduce risks. This article explores the latest developments in the treatment of multinodular goitre.
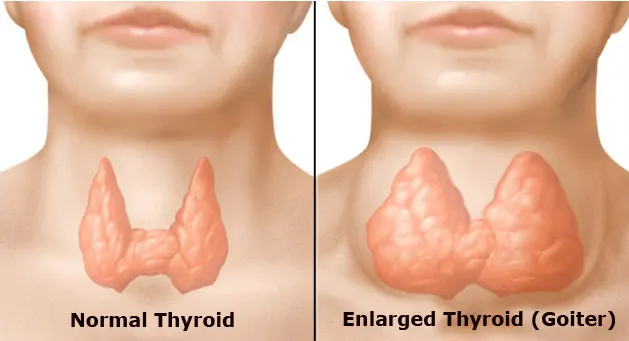
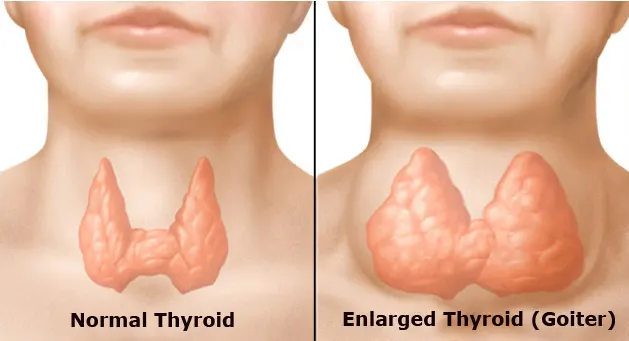
Understanding Multinodular Goitre
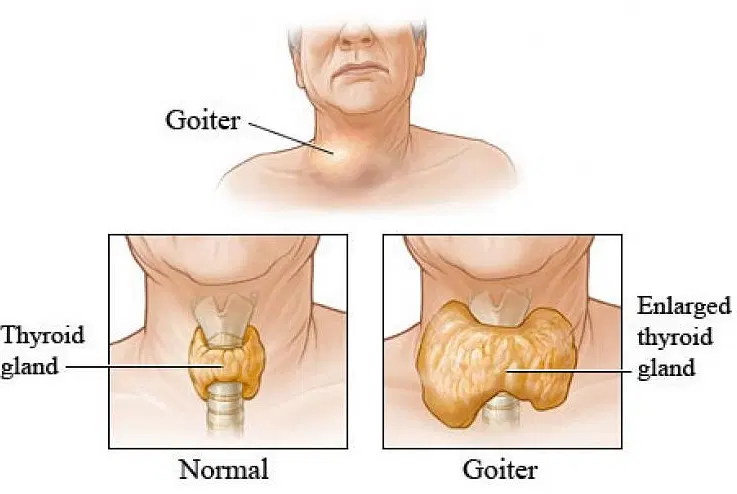
To appreciate the advancements in treatment, it is essential to understand the nature of multinodular goitre. Hormones that control metabolism are produced by the thyroid gland, which is situated near the base of the neck. In MNG, the thyroid enlarges due to the presence of multiple nodules, which can vary in size and function. These nodules may be benign or malignant and can cause symptoms such as neck swelling, difficulty swallowing, and hormonal imbalances.
Traditional Treatment Approaches
Historically, the primary treatments for MNG have been surgical removal of the thyroid gland (thyroidectomy) and radioactive iodine (RAI) therapy. Surgery is typically reserved for large goitres causing compressive symptoms or when malignancy is suspected. RAI therapy, on the other hand, is used to reduce the size of the goitre and manage hyperthyroidism. While effective, these treatments come with potential risks and side effects, prompting the search for alternative approaches.
Minimally Invasive Surgical Techniques
One significant advancement in the treatment of MNG is the development of minimally invasive surgical techniques. Traditional thyroidectomy involves a large incision in the neck, leading to scarring and longer recovery times. In contrast, minimally invasive procedures, such as endoscopic and robotic-assisted thyroidectomy, require smaller incisions and offer several benefits:
- Reduced Scarring: Smaller incisions result in less noticeable scars, which is a significant cosmetic advantage for patients.
- Shorter Recovery Time: Minimally invasive techniques typically result in quicker recovery compared to traditional surgery.
- Lower Risk of Complications: These procedures reduce the risk of complications such as damage to the parathyroid glands and recurrent laryngeal nerve.
Radiofrequency Ablation (RFA)
Radiofrequency ablation (RFA) is a non-surgical treatment option that has gained popularity in recent years. RFA uses heat generated by radiofrequency energy to destroy thyroid nodules. This technique is particularly effective for benign nodules and offers several advantages:
- Minimally Invasive: RFA is performed under local anesthesia with a small needle, minimizing the need for large incisions.
- Outpatient Procedure: Patients can typically return home the same day, making it a convenient option.
- Low Risk of Complications: RFA has a low complication rate, preserving thyroid function and reducing the risk of damage to surrounding structures.
Ethanol Ablation
Ethanol ablation, also known as percutaneous ethanol injection (PEI), is another minimally invasive technique used to treat thyroid nodules. This method involves injecting ethanol directly into the nodule, causing it to shrink. Ethanol ablation is particularly effective for cystic and predominantly cystic nodules. Key benefits include:
- Non-surgical: PEI is performed using a fine needle, eliminating the need for surgery.
- Effective for Cystic Nodules: Ethanol ablation is highly effective in reducing the size of cystic thyroid nodules.
- Quick Recovery: Patients can resume normal activities shortly after the procedure.
Advances in Radioactive Iodine Therapy
While radioactive iodine therapy has been a mainstay in the treatment of MNG, advancements have improved its efficacy and safety. Recent developments include:
- Personalized Dosing: Advances in imaging and dosimetry allow for personalized RAI dosing, optimizing treatment efficacy while minimizing side effects.
- Adjunctive Medications: The use of medications such as recombinant human thyrotropin (rhTSH) can enhance the effectiveness of RAI therapy by stimulating iodine uptake by the thyroid gland.
Targeted Molecular Therapies
Research into the molecular mechanisms underlying thyroid nodules has led to the development of targeted therapies. These treatments aim to address the specific genetic mutations and pathways involved in nodule formation and growth. Examples include:
- Tyrosine Kinase Inhibitors (TKIs): TKIs target specific proteins involved in thyroid cell growth and proliferation. These drugs have shown promise in treating advanced thyroid cancers and may have applications in managing benign nodules.
- Gene Therapy: Advances in gene therapy hold the potential to correct genetic mutations responsible for nodule development, offering a more targeted and long-term solution.
Monitoring and Follow-Up
Advancements in imaging technology have improved the ability to monitor and follow up with patients with MNG. High-resolution ultrasound, elastography, and advanced imaging techniques provide detailed information about nodule size, composition, and vascularity. These tools enable:
- Accurate Assessment: Improved imaging allows for accurate assessment of nodule characteristics and changes over time.
- Early Detection of Malignancy: Advanced imaging can help detect malignant changes in nodules at an early stage, facilitating timely intervention.
- Tailored Treatment Plans: Detailed imaging data allows for more personalized treatment plans based on individual nodule characteristics.
Conclusion
Advancements in the treatment of multinodular goitre have significantly improved patient outcomes and quality of life. Minimally invasive surgical techniques, radiofrequency and ethanol ablation, personalized radioactive iodine therapy, and targeted molecular treatments offer effective alternatives to traditional approaches. Additionally, advances in imaging technology have enhanced the ability to monitor and manage MNG, ensuring timely and tailored interventions. As research continues, these innovations promise to further refine and expand the options available for patients with multinodular goitre, offering hope for improved management and better overall health outcomes.