Thyroiditis In Children And Adolescents: Special Considerations
Thyroiditis, an inflammation of the thyroid gland, is a condition that can affect individuals of all ages, including children and adolescents. While thyroiditis in this demographic group shares similarities with the condition in adults, there are also unique considerations and challenges. Understanding these special considerations is crucial for accurate diagnosis, appropriate management, and optimal outcomes in pediatric patients. This article delves into the distinct features of thyroiditis in children and adolescents, covering its prevalence, causes, clinical presentation, diagnosis, treatment, and long-term implications.
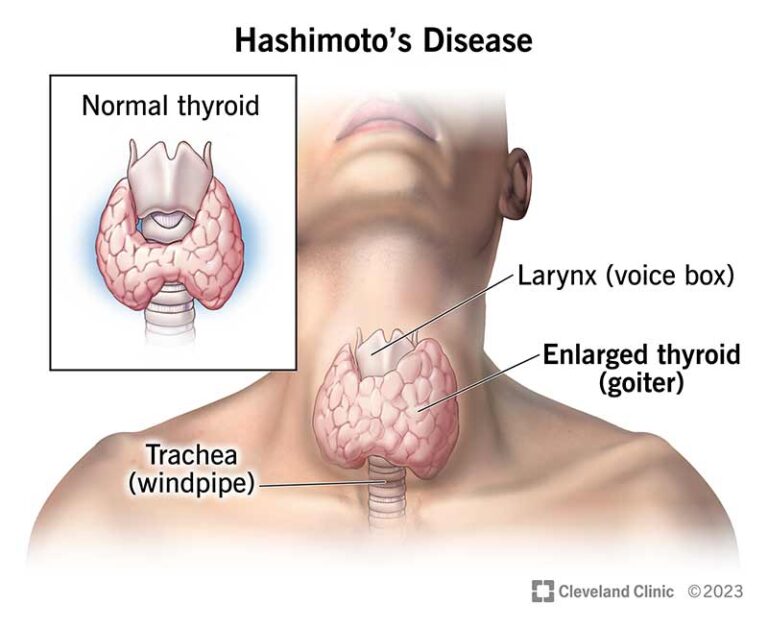
Prevalence and Causes
Thyroiditis in children and adolescents is relatively rare compared to adults, but it can still occur. The most common types of thyroiditis in this age group include Hashimoto’s thyroiditis, subacute thyroiditis, and postpartum thyroiditis (when it occurs in adolescents). Hashimoto’s thyroiditis, an autoimmune condition characterized by chronic inflammation of the thyroid gland, is the predominant cause of hypothyroidism in children and adolescents. Subacute thyroiditis, often triggered by a viral infection, can also occur in this age group, albeit less frequently.
Clinical Presentation
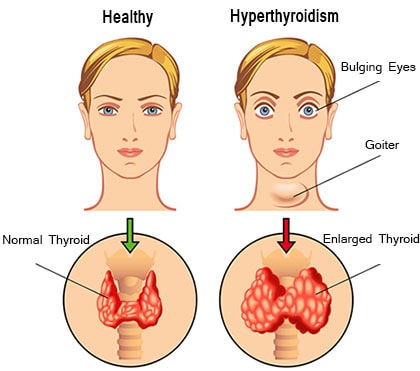
The clinical presentation of thyroiditis in children and adolescents may vary depending on the underlying cause and stage of the disease. In Hashimoto’s thyroiditis, symptoms of hypothyroidism, such as fatigue, weight gain, cold intolerance, constipation, and delayed growth and development, may manifest gradually over time. In contrast, subacute thyroiditis typically presents with symptoms of hyperthyroidism initially, including palpitations, heat intolerance, weight loss, and irritability, followed by transient hypothyroidism as the inflammation resolves.
Diagnosis
Diagnosing thyroiditis in children and adolescents requires a comprehensive evaluation that includes a thorough medical history, physical examination, and laboratory testing. Laboratory tests commonly performed to assess thyroid function include measurement of thyroid-stimulating hormone (TSH), free thyroxine (T4), and thyroid peroxidase antibodies (TPOAb). Imaging studies, such as thyroid ultrasound, may also be employed to assess the size and appearance of the thyroid gland and detect abnormalities suggestive of thyroiditis.
Treatment
The management of thyroiditis in children and adolescents aims to alleviate symptoms, restore thyroid function to normal levels, and prevent complications. In Hashimoto’s thyroiditis, treatment typically involves thyroid hormone replacement therapy with levothyroxine to supplement deficient thyroid hormone levels and normalize thyroid function. Regular monitoring of thyroid function tests is essential to adjust medication dosages as needed and ensure optimal thyroid hormone levels. In cases of subacute thyroiditis, symptomatic relief with nonsteroidal anti-inflammatory drugs (NSAIDs) may be sufficient, although beta-blockers may be prescribed to alleviate symptoms of hyperthyroidism if necessary.
Long-term Implications
Thyroiditis in children and adolescents can have long-term implications for growth, development, and overall health if left untreated or inadequately managed. Untreated hypothyroidism resulting from Hashimoto’s thyroiditis can lead to growth retardation, delayed puberty, cognitive impairment, and other developmental issues. Conversely, untreated hyperthyroidism secondary to subacute thyroiditis can result in complications such as cardiac arrhythmias, osteoporosis, and thyroid storm, a life-threatening condition characterized by severe hyperthyroidism.
Special Considerations
In addition to standard diagnostic and treatment approaches, several special considerations apply to the management of thyroiditis in children and adolescents. Pediatric patients may require individualized dosing of thyroid hormone replacement therapy based on age, weight, and growth parameters to ensure adequate hormone replacement and promote normal growth and development. Furthermore, regular monitoring of thyroid function and growth parameters is essential to assess treatment response, detect complications, and optimize long-term outcomes.
Conclusion
Thyroiditis in children and adolescents presents unique challenges and considerations that differ from those in adults. Recognizing the distinct clinical features, diagnostic criteria, and treatment approaches for thyroiditis in this age group is essential for providing optimal care and achieving favorable outcomes. By addressing the special considerations outlined in this article, healthcare providers can effectively manage thyroiditis in pediatric patients and support their growth, development, and overall well-being.